January 2026
A policy brief prepared by UConn School of Pharmacy, Connecticut Pharmacists Association (CPA), Connecticut Community Pharmacy Enhanced Services Network (CPESN), UConn Health Pharmacy Department, Yale New Haven Pharmacy Department
CONTACTS:
Marie Smith, Assistant Dean, UConn School of Pharmacy, marie.smith@uconn.edu
Nathan Tinker, CEO, Connecticut Pharmacists Association, ntinker@ctpharmacists.org
OVERVIEW
With the Connecticut Rural Health Transformation (RHT) program funding, we recommend that the design of new care delivery and payment models should incorporate collaborative, team-based pharmacist practice models described below – embedded pharmacists in primary care offices, clinics, and FQHCs; community pharmacists with remote monitoring capability, and e-consult pharmacists. These models, if adequately supported with RHT funding, can improve population health outcomes, workforce shortages, care coordination, and high-quality care in CT’s rural communities.
As mentioned in the CT RHT Program application, pharmacists need to be members of care teams in primary care offices, outpatient clinics, and FQHCs for medication optimization and management of medication-related chronic conditions such as hypertension, diabetes, and chronic kidney disease. It has been estimated that over 500 billion dollars is wasted and 275,000 lives are lost each year in the United States due to non-optimized medication use.
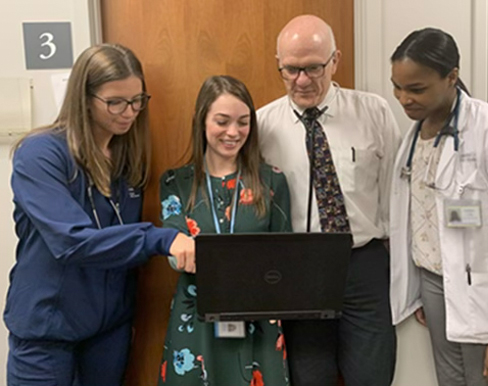
Since 2019, CT pharmacists have had collaborative practice authority with physicians and APRNs to optimize and manage medications, thereby reducing the workload and increasing the efficiency of time-constrained PCPs. UConn School of Pharmacy research demonstrated that 1 FTE pharmacist using collaborative practice agreements in a primary care office can save 640 physician hours/year on medication management activities. This can open up 1,920 patient appointments per year to improve both patient access and PCP workforce shortage issues.
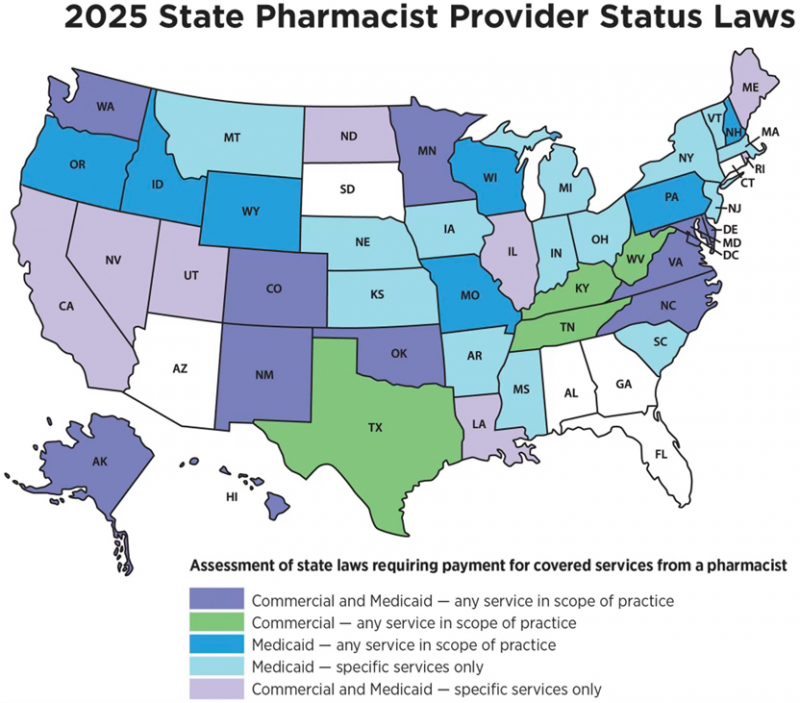
Today, CT pharmacists are highly trained yet underutilized in primary care roles due to the lack of a sustainable payment model. As of November 2025, CT is one of six states without any pharmacist payment model. Nearly 40 state Medicaid programs recognize pharmacists as Medicaid providers with payment for all or some medication optimization and management (non-dispensing) services. In February 2024, the CMS Administrator clarified that states can enroll pharmacists as Medicaid providers through the Other Licensed Practitioner benefit. Several states have submitted State Plan Amendments to enroll pharmacists as providers.
RHT INITIATIVES
As CT implements its four major RHT initiatives, we offer current examples of pharmacist practice models and programs that can be expanded and replicated in rural communities.

Population Health – embedded pharmacist collaborative practice models exist in several CT primary care teaching sites (i.e., UConn Health, Yale Health, Hartford HealthCare, FQHCs) that can be replicated in RHT designated areas. In addition, the Community Pharmacy Enhanced Services Network (CPESN) — 28 independent community pharmacies throughout CT — provide additional patient access points for chronic medication optimization, management, and monitoring. There are 600 community pharmacies in CT – including 25 in northeastern CT and 19 in northwestern CT – who are ready to work with the RHT program and patients with uncontrolled hypertension, diabetes, and chronic kidney disease.
In the 2010 CT Medicaid Transformation project, pharmacists collaborating with PCPs and Medicaid patients in FQHCs showed a 28% increase in achievement of BP and A1c goalswithin 6 months when patient-pharmacist visits were scheduled between regular PCP appointments.
Workforce Development – pharmacists in UConn School of Pharmacy, UConn Health, Hartford HealthCare, and Yale Health are mitigating primary care workforce shortages.
Pipeline and Upskilling: UConn School of Pharmacy trains nearly 400 Doctor of Pharmacy students/year, participates in statewide recruitment events (e.g., career fairs, summer camps, high school guidance counselor visits), and provides over 60,000 hours/year of pharmacist continuing professional education to upskill current pharmacists for rural health needs.
Embedded and Telehealth Pharmacists: 5 UConn School of Pharmacy faculty members practice in primary care practices/clinics at Hartford HealthCare Integrated Care Partners, St. Francis Asylum Hill Family Medicine Program, Brownstone Clinic, and UConn Health Internal Medicine Clinic.
Hartford HealthCare Medical Group (HHCMG) has 3 embedded primary care pharmacists serving 13 of 70 offices in Enfield, Bloomfield, Windsor, South Windsor, Manchester, Vernon, Southington and Plainville. After 6 months of success, HHCMG is expanding this pharmacist program to additional high need areas. Also, HHCMG in partnership with UConn School of Pharmacy received a grant from the American Association of Psychiatric Pharmacists to add 3 behavioral health pharmacist specialists in Bridgeport, Windham and one additional location.

Yale New Haven Health has 2 pharmacists working in Bridgeport Hospital Primary Care Clinic that serves an indigent patient population, and 8 pharmacists centrally support referrals from over 50 Northeast Medical Group primary care practices and 1 Yale Medicine Primary Care practice through telehealth services for chronic disease management.
Pharmacy residencies: there are 20 PGY1 pharmacy residency programs in CT and 4 PGY2 ambulatory care pharmacy residencies (UConn Health, Hartford HealthCare, Yale New Haven Hospital, St. Francis) that could be expanded for training in rural health areas. UConn Health may expand pharmacy residencies in rural areas with the acquisition of Day Kimball/Waterbury Hospitals.
These current embedded pharmacist and pharmacy residency training programs can be considered for expansion or replication into rural CT regions with RHT funding –- creates innovative practice opportunities, addresses PCP shortages, improves population health programs, and trains medical and pharmacy students/residents on sustainable team-based workforce models.
Data and Technology – Health Information Exchange (HIE) patient-level medication lists are often incomplete, inaccurate, and not current. Also, pharmacists are underutilized in remote monitoring and e-consult initiatives.
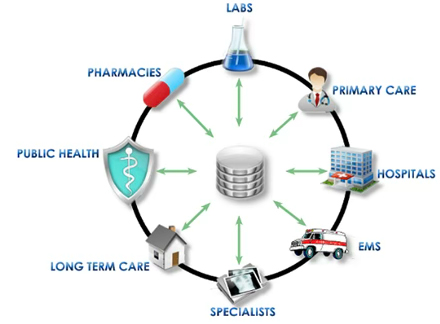
Health Information Exchange: CT’s HIE, Connie, is not interoperable with over 600 pharmacies in CT, which leaves community-based pharmacists unable to access hospital admission and discharge info, lab reports, and medication lists for the patients they serve. Pharmacy information systems should be able to add real-time data for new, changed, or discontinued medications, and vaccinations administered so there is a shared repository for a patient’s medication information.
While community pharmacies manage 83% of prescription volume, more prescriptions are being delivered through alternative channels — online, specialty, mail-order, home infusion, compounding, hospital, free clinic pharmacies; and direct-to-consumer channels that usually are not connected to HIEs. So, all pharmacies and other medication sources need to be connected to Connie for pharmacist access to necessary patient info, as well as uploading current medication info to Connie databases. Without a consolidated and accurate medication list available to patients’ providers, clinical decision-making may be misinformed and result in patient harm (e.g., drug interactions, adverse drug events, duplicate therapy).

Remote monitoring: pharmacists should be included in remote monitoring and management programs for patients with uncontrolled chronic diseases such as hypertension, diabetes, and congestive heart failure. All of these conditions can be monitored with digital monitoring devices at home (i.e., blood pressure cuff, glucose meter, and scale). Undertreatment may be especially problematic in medically unserved rural areas with reduced access to medical care. In a survey of CT providers, 79% of PCPs agreed that community pharmacists could provide useful medication monitoring reports and actionable recommendations between PCP visits to improve clinical outcomes for patients with hypertension and diabetes. As CT moves to more value-based payment arrangements, community-based pharmacists can help PCPs achieve quality care metrics and performance-based payments by providing patient access between PCP appointments.
E-consults: in rural areas without embedded pharmacists, an alternative model of pharmacists in e-consult networks as pharmacotherapy specialists should be considered with RHT program funding. In CT, more than 90% of primary care practices do not have clinical pharmacists as members of expanded care teams. The emergence of e-consult services presents an opportunity for PCPs in rural areas to consult with pharmacists as “on-demand” pharmacotherapy specialists. A UConn School of Pharmacy demonstration project showed that e-consults are feasible between PCPs and pharmacists; medication-related questions came from both APRNs and physicians without an embedded pharmacist.
CARE TRANSFORMATION AND SUSTAINABILITY
As the RHT program implements value-based payment programs, a successful example can be a collaborative pharmacist care model in the CT Medicaid Transformation Program that demonstrated cost savings. Pharmacists in FQHCs identified and resolved nearly 80% of all medication-related problems after 4 pharmacist-patient encounters. We used a total cost of care model to assess the cost impact of pharmacist-provided intensive medication optimization services described above. Key findings were:
• An estimated annual saving of $1,595 per patient – approximately a 3:1 ROI for the embedded pharmacist services. Savings were $1,123 per patient/year on medication claims and $472 per patient/year on medical, hospital, and emergency department expenses. Medication cost reductions were attained by reducing unnecessary, duplicate, or discontinued meds; eliminating meds with adverse effects; titrating to effective doses; and using more cost-effective therapies.
• Using actual Medicaid claims data, cost reductions for 12 months pre- and post-pharmacist medication optimization services were a 23% reduction for drug costs, 42% decrease in hospital costs, and a 29% reduction of emergency room costs.
TECHNICAL ASSISTANCE EXPERTISE
UConn School of Pharmacy has technical assistance experience with 2 CMS projects and stands ready to contract with the RHT Program implementation process for team-based pharmacist and payment reform initiatives:
CT Medicaid Transformation Program (2009-2010): developed an integrated pharmacist model in a statewide FQHC for comprehensive medication management interventions with Medicaid patients to demonstrate improved patient outcomes and total cost of care savings.
CMS State Innovation Model Technical Assistance Program on Primary Care Pharmacist Integration (2019-2020): provided tailored technical assistance for high-impact integration of pharmacists in 4 large primary care organizations (Community Health Center Inc., Nuvance, Yale/Northeast Medical Group, Prospect Medical ACO). The program involved facilitating interdisciplinary discussions to identify high-value/high-impact patients, and organizational priorities for pharmacist medication optimization and management services. Clinical leaders and PCPs were provided information on various pharmacist service models (e.g., direct patient care, population health, and co-visits) and participated in the design of short-term pilot projects to demonstrate pharmacist impact.
CONCLUSION
Connecticut’s Rural Health Transformation Program offers a rare and timely opportunity to strengthen care delivery, expand workforce capacity, and achieve measurable improvements in population health — particularly in rural and medically underserved communities. Pharmacists represent an immediately available, highly trained, and cost-effective resource that can be deployed through embedded care models, community-based services, remote monitoring, and e-consult networks. By explicitly incorporating pharmacist services and sustainable payment pathways into RHT program design, the state can leverage existing infrastructure, academic partnerships, and demonstrated return-on-investment to accelerate impact. Integrating pharmacists is not an incremental adjustment but a strategic multiplier that will enhance team-based care, improve medication outcomes, and ensure that RHT investments deliver durable, statewide value for patients, providers, and payers alike.
